- COVID-19 travel advice
Lower your risk of COVID-19 as you travel for a safe and fun adventure.
Successful travel starts with being prepared for the unexpected. Coronavirus disease 2019, known as COVID-19, is now a part of standard travel planning.
As you choose a destination, travel group or event, add COVID-19 to the list of things to research. When packing for yourself or anyone you're caring for on the trip, consider COVID-19 prevention and testing.
No one wants to plan for the worst. But having a plan in case you catch the COVID-19 virus while traveling can save time if you need medical care.
To start, it can help to ask these basic questions as you make plans.

Am I up to date with my COVID-19 vaccine?
Staying up to date on your COVID-19 vaccine helps prevent serious illness, the need for hospital care and death due to COVID-19 .
If you need a vaccine, plan to get it at least a few weeks before you travel. Protection from the vaccine isn't immediate.
Am I, a travel companion or a person I live with at high risk of serious COVID-19 illness?
Many people with COVID-19 have no symptoms or mild illness. But for older adults and people of any age with certain medical conditions, COVID-19 can lead to the need for care in the hospital or death.
If you or those around you are at high risk of serious COVID-19 illness, take extra safety measures during or after travel.
Ask a healthcare professional if there are any specific actions you should take.
Does my destination, tour group or event need proof that I had a COVID-19 vaccine? Do I need to show proof of a negative COVID-19 test?
The country you travel to may not need to know your COVID-19 status. But you might need the information for other reasons.
Events, venues or tour groups might require proof that you are COVID-19 negative or are up to date on a COVID-19 vaccine. Check before you go so you have all the paperwork you need.
What's the plan if I get COVID-19 on my trip?
No one wants to get sick while traveling. But in case you do, it helps to know where you can get medical care and whether you'll be able to stay apart from others while you have symptoms.
Put together a COVID-19 kit with rapid home tests, masks, a thermometer, disinfectant wipes and hand sanitizer that contains at least 60% alcohol.
Before you leave, gather health information from your healthcare professional. Make sure it gives the details on any health conditions you're managing and medicine you take.
COVID-19 spread during travel
The virus that causes COVID-19 spreads mainly from person to person. When the virus is spreading, spending time indoors with a crowd of people raises your risk of catching it. The risk is higher if the indoor space has poor airflow.
The coronavirus is carried by a person's breath.
The virus spreads when a person with COVID-19 breathes, coughs, sneezes, sings or talks. The droplets or particles the infected person breathes out could possibly be breathed in by other people if they are close together or in areas with low airflow.
The virus carried by a person's breath can land directly on the face of a nearby person, after a sneeze or cough, for example. And people may touch a surface that has respiratory droplets and then touch their faces with hands that have the coronavirus on them.
Clean hands
While you travel, one way to lower your risk of COVID-19 is to clean your hands often.
Wash your hands after using the bathroom, before making food or eating, and after coughing, sneezing or blowing your nose. If you touch something that others regularly touch, such as an elevator button or a handrail, make sure to clean your hands afterward.
Also, try to avoid touching your eyes, nose or mouth.
Wearing a face mask is another way to lower your risk of COVID-19 .
Travel brings people together from areas where viruses may be spreading at higher levels. Masks can help slow the spread of respiratory viruses in general, including the COVID-19 virus.
Masks help the most in places with low airflow and where you are in close contact with other people. Also, masks can help if viruses are spreading at high levels in the places you travel to or through.
Masking is especially important if you or a companion have a high risk of serious COVID-19 illness. Choose the most protective mask that fits well and is comfortable.
Get the COVID-19 vaccine
As the virus that causes COVID-19 changes, COVID-19 vaccines are updated, so stay up to date with the recommended shots.
Know when the COVID-19 virus is spreading in your area
Check with health agencies in the area to see where the COVID-19 virus is spreading. Information about the spread of the virus may include the number of people in the hospital with COVID-19 or the number of people who test positive for the disease.
Keep some space around you
Choose outdoor activities and keep some distance between yourself and others. Poor airflow plus lots of people crowded together equals a higher chance you'll come in contact with the virus that causes COVID-19 .
If you can, try to avoid spending time with people who have COVID-19 symptoms or who are sick.
There will likely be times during travel when you don't have a choice about how close you are to others. Here are some tips for air travel, public transportation and lodging.
The risk of catching the virus that causes COVID-19 from air travel is thought to be low.
Air in the plane's cabin changes over quickly during the flight, being replaced every few minutes in some planes. Airplane air also is often filtered. So germs, including viruses, are trapped before they spread.
The air flowing down from vents above the seats in each row may help keep germs from spreading. Seats also may act as a barrier to germ spread on a plane, unless the person who is ill is sitting close to you.
You can help lower your risk by spreading out to keep distance between you and others when you can and cleaning your hands regularly.
Wearing a mask in crowded areas, such as security lines and bathrooms, can help protect you from COVID-19 and other respiratory illnesses.
Trains, buses and cars
Trains and buses may have good airflow and air filtering. But check before you travel so you know what to expect. When a vehicle is crowded, wear a face mask and take other steps, such as cleaning your hands.
Taxis and private cars used for ride-sharing may not have air filtering. But in most cases, rolling down a window could be an option to improve airflow.
Rental car companies may post their cleaning policies on the internet, or you can ask directly when you book the vehicle.
Hotels and other lodging
Cleaning protocols at hotels, vacation rentals and other lodging have largely returned to the way they were before the COVID-19 pandemic. If you have questions about how hosts or businesses protect guests, contact them directly. In public areas of hotels, take steps to lower your risk of catching the virus that causes COVID-19 .
Put safety first
Despite your planning, an illness may delay or cancel your trip. Stay home if you or anyone you're traveling with has:
- Symptoms of COVID-19 , such as fever or new loss of taste or smell.
- Taken a COVID-19 test and is waiting for results.
- Been diagnosed with COVID-19 .
Keep watch for serious symptoms of COVID-19 , such as trouble breathing or chest pain. If you or a person you're taking care of has symptoms that worry you, get help.
Once the fever is gone and symptoms are getting better, you may choose to travel. But for about five days after feeling better, you could still give others the virus that causes COVID-19 . Take extra actions to protect the people around you.
- Wear a mask.
- Keep your distance from others, especially when indoors.
- Clean your hands regularly.
- Keep the air flowing by turning on fans or opening windows when you can.
If you start to feel worse or your fever comes back, avoid being around others again until you feel better.
Stay flexible
With COVID-19 vaccinations, testing and treatment, events and travel are back to typical levels in many places. But as waves of COVID-19 outbreaks happen, it's important to stay flexible with your plans. Knowing whether the COVID-19 virus is spreading in your area or in places where you're traveling can help you make decisions about whether to go and what to put on your agenda.
- Stay up to date with COVID-19 vaccines. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/stay-up-to-date.html. Accessed May 15, 2024.
- Understanding how COVID-19 vaccines work. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/how-they-work.html. Accessed May 15, 2024.
- People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed May 15, 2024.
- Coronavirus disease (COVID-19): Travel advice for the general public. World Health Organization. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/coronavirus-disease-covid-19-travel-advice-for-the-general-public. Accessed May 15, 2024.
- Centers for Disease Control and Prevention. COVID-19. In: CDC Yellow Book 2024. https://wwwnc.cdc.gov/travel/yellowbook/2024/infections-diseases/covid-19. Accessed May 15, 2024.
- Centers for Disease Control and Prevention. Obtaining health care abroad. In: CDC Yellow Book 2024. https://wwwnc.cdc.gov/travel/yellowbook/2024/health-care-abroad/health-care-abroad. Accessed May 15, 2024.
- Goldman L, et al., eds. COVID-19: Epidemiology, clinical manifestations, diagnosis, community prevention, and prognosis. In: Goldman-Cecil Medicine. 27th ed. Elsevier; 2024. https://www.clinicalkey.com. Accessed May 16, 202.
- Taking steps for cleaner air for respiratory virus prevention. Centers for Disease Control and Prevention. https://www.cdc.gov/respiratory-viruses/prevention/air-quality.html. Accessed May 16, 2024.
- How COVID-19 spreads. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid-spreads.html. Accessed May 16, 2024.
- COVID-19 overview and infection prevention and control priorities in non-U.S. healthcare settings. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/overview/index.html. Accessed May 16, 2024.
- Hygiene and respiratory viruses prevention. Centers for Disease Control and Prevention. https://www.cdc.gov/respiratory-viruses/prevention/hygiene.html. Accessed May 14, 2024.
- About handwashing. Centers for Disease Control and Prevention. https://www.cdc.gov/clean-hands/about/index.html. Accessed May 16, 2024.
- Masking during travel. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/page/masks. Accessed May 16, 2024.
- Masks and respiratory virus prevention. Centers for Disease Control and Prevention. https://www.cdc.gov/respiratory-viruses/prevention/masks.html. Accessed May 16, 2024.
- How to protect yourself and others. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html. Accessed May 16, 2024.
- About physical distancing and respiratory viruses. Centers for Disease Control and Prevention. https://www.cdc.gov/respiratory-viruses/prevention/physical-distancing.html. Accessed May 16, 2024.
- How can ventilation reduce the risk of contracting COVID-19 on airplanes? World Health Organization. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/coronavirus-disease-covid-19-travel-advice-for-the-general-public. Accessed May 16, 2024.
- Bielecki M, et al. Air travel and COVID-19 prevention in the pandemic and peri-pandemic period: A narrative review. Travel Medicine and Infectious Disease. 2021; doi:10.1016/j.tmaid.2020.101915.
- Symptoms of COVID-19. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html. Accessed May 16, 2024.
- Preventing spread of respiratory viruses when you're sick. Centers for Disease Control and Prevention. https://www.cdc.gov/respiratory-viruses/prevention/precautions-when-sick.html. Accessed May 16, 2024.
Products and Services
- A Book: Endemic - A Post-Pandemic Playbook
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- A Book: Future Care
- Antibiotics: Are you misusing them?
- COVID-19 and vitamin D
- Convalescent plasma therapy
- Coronavirus disease 2019 (COVID-19)
- COVID-19: How can I protect myself?
- Herd immunity and respiratory illness
- COVID-19 and pets
- COVID-19 and your mental health
- COVID-19 antibody testing
- COVID-19, cold, allergies and the flu
- COVID-19 tests
- COVID-19 drugs: Are there any that work?
- COVID-19 in babies and children
- Coronavirus infection by race
- COVID-19 vaccine: Should I reschedule my mammogram?
- COVID-19 vaccines for kids: What you need to know
- COVID-19 vaccines
- COVID-19 variant
- COVID-19 vs. flu: Similarities and differences
- COVID-19: Who's at higher risk of serious symptoms?
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Extracorporeal membrane oxygenation (ECMO)
- Fever: First aid
- Fever treatment: Quick guide to treating a fever
- Fight coronavirus (COVID-19) transmission at home
- Honey: An effective cough remedy?
- How do COVID-19 antibody tests differ from diagnostic tests?
- How to measure your respiratory rate
- How to take your pulse
- How to take your temperature
- How well do face masks protect against COVID-19?
- Is hydroxychloroquine a treatment for COVID-19?
- Long-term effects of COVID-19
- Loss of smell
- Mayo Clinic Minute: You're washing your hands all wrong
- Mayo Clinic Minute: How dirty are common surfaces?
- Multisystem inflammatory syndrome in children (MIS-C)
- Nausea and vomiting
- Pregnancy and COVID-19
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- Sex and COVID-19
- Shortness of breath
- Thermometers: Understand the options
- Treating COVID-19 at home
- Unusual symptoms of coronavirus
- Vaccine guidance from Mayo Clinic
- Watery eyes
Related Information
- Coronavirus: What is it and how can I protect myself?
- COVID-19 vaccines: Get the facts
- COVID-19 , cold, allergies and the flu: What are the differences?
5X Challenge
Thanks to generous benefactors, your gift today can have 5X the impact to advance AI innovation at Mayo Clinic.
- Skip to main content
- Keyboard shortcuts for audio player
Goats and Soda
- Infectious Disease
- Development
- Women & Girls
- Coronavirus FAQ
Coronavirus, Illustrated
Coronavirus faq: i took a trip and caught covid. what should i do when can i go home.

Marc Silver

We regularly answer frequently asked questions about life during the coronavirus crisis. If you have a question you'd like us to consider for a future post, email us at [email protected] with the subject line: "Weekly Coronavirus Questions." See an archive of our FAQs here .
I flew away on a trip ... and I caught COVID. Now what?
So you've joined the millions of travelers who are taking off this summer, headed for vacations, weddings, family reunions, conferences. And you flew to your destination.
You arrive, you're having a great time. Then you feel a little off. Your throat is scratchy. Maybe you start coughing. Or your head feels as if it is about to float off your body like a rogue balloon.
Sigh. Time for a COVID test. The bad news: You're positive!
What do you do now? Where do you stay? Can you score some Paxlovid if you're a good candidate for this or another anti-COVID drug? And the big question: When can you fly home? True confession: It happened to me. Here's what I learned from the experience and from interviews afterward with COVID experts.
Prepare for COVID before the trip starts
Actually, the first question is: Did you prepare for a possible COVID case before taking off?
Any traveler who has yet to go on a summer trip needs to keep in mind that the pandemic is still going on. Surges are happening across the U.S. and in popular tourist destinations like France, Italy and Spain.
That means your trip planning can't just focus on what to see and where to eat. You need to think about COVID prep, too. The COVID experts we interviewed suggest these pre-trip steps:
- Pack self-tests and high quality (N95 or KN95) masks. Because you sure don't want to have to hunt them down in an unfamiliar place. Also: bring along a thermometer and pulse oximeter so you can monitor your health should you get infected.
- Make sure you have easy access to your online medical records. In the event you need to seek antiviral treatments, the prescriber needs this info to determine if you have any health issues or are taking medications that might cause problems if you start a Paxlovid regimen.
- If you're eligible for a booster, roll up your sleeve before departing. It's not ironclad protection against infection but could mean a less severe course of disease.
- If you're going out of the country, consider buying travel insurance. A policy can ensure that you can get care in a foreign country or a medical evacuation if need be.
- Check to see if your destination country has any COVID testing requirements for arrivals or departures. (The U.S. last month dropped its requirement that arrivals from other countries test for COVID.) But finding out the rules and regs in another country can be tough – websites can't always keep up with all the updates, notes Dr. Henry Wu , a professor of infectious disease medicine at Emory University and director of its TravelWell Center. A tour operator or hotel where you plan to stay might be a good pre-trip source if you strike out in your hunt for official info online.
- Brush up on local medical source. If you're in a country that doesn't have a strong health care infrastructure or is in a remote area, see if you can get the answer to this question from a local source in advance, Wu suggests: Where should I call if I become really sick?
- Be prepared financially. You'll want to put aside some extra money for your trip if COVID strikes, to spend on additional nights at a hotel and unexpected health-care and other costs.
- Finally, if you know anyone at your destination, touch base with them before departing. They could be your guardian angel if you need a COVID assist. Make sure you have their contact details in case of emergency.
What to do when you get that positive test
Now, back to our drama: I went on vacation and all I got was a lousy case of COVID!
When you find out you've got COVID, the Centers for Disease Control and Prevention has this recommendation: "Do not travel until a full 10 days after your symptoms started or the date your positive test was taken if you had no symptoms ." The goal is to keep you from infecting others while you are still contagious.
So you'll have two types of concerns: rearranging your travel plans – and figuring out when you can return home.

Coronavirus FAQ: Should I still take a COVID test before flying into the U.S.?
First, let's consider the immediate logistics.
Where will you stay?
You can try to extend the course your current lodging. Hotel representatives we interviewed suggest asking the property if they're open to a guest who's isolating with COVID. A hotel that says yes will probably also tell you that there will be no housekeeping services — but you can ask for towels, room service or food dropped off from a delivery app to be left outside your door (which should have the "do not disturb" sign on the knob at all times). If the hotel isn't open to hosting a guest with COVID or your room just isn't available, look for a new lodging option.
Uh-oh. My rental car is due back!
Unless you can drop it off in a contact-free situation and walk back to your isolation lodging, you've got a dilemma. Fortunately, rental car companies understand. Really. Of course, different companies have different options. Gabriel, a very helpful customer service rep for Avis, says that depending on the circumstances, his company might send a team to pick up the car, arrange for a tow or authorize another driver to return the car. Or if you want to hold onto the car until you're recovered, they might be able to extend your rental, perhaps at a reduced rate given the circumstances.
If all else fails, you can rely on the kindness of others. When I found myself in this situation, my daughter's friend's boyfriend offered to return our car – about an hour's drive. I paid for his Uber back but he wouldn't take a penny for his good deed. As my daughter's friend put it, "being sick [is] a tricky pickle to be in right now. We would love to help."
Getting Paxlovid (or another antiviral treatment)
Even if you'd like to bring a precautionary stash of the drug on your trip, you are not allowed to do so by the terms of the Food and Drug Administration's emergency use authorization for Pfizer's Paxlovid pill , which is recommended for people at risk of severe disease, like older folks or those with certain medical conditions.

Coronavirus FAQ: I took Paxlovid. I felt better. Then symptoms rebounded. What's up?
But time is of the essence with Paxlovid. You want to start your twice-daily dose of three tablets within 5 days of testing positive. You can contact your primary care physician and give them the name of a local pharmacy. Or you can Google a telehealth portal that will take your info and put in a prescription. That could cost around $75 for the service. Or you can take advantage of the brand-new FDA ruling. Not every pharmacy is on board, but pharmacies that offer "test to treat" services are a likely option. Check out the Department of Health & Human Services' online locator tool to find participating pharmacies.
And, um, how do you get the prescription if you have COVID? The pharmacy I used told me, "You know you CANNOT COME IN to pick up the pill because you have COVID." Some pharmacies do have delivery or drive-through options. If you have a family member or friend at your destination, ask a favor. If you're out of options, you could turn to an online service like TaskRabbit, which can help you find someone to hire to run an errand for you.
If the only alternative is picking it up yourself, says Dr. Jill Weatherhead , assistant professor of adult and pediatric infectious diseases at Baylor College of Medicine, "make sure you have on a KN95 or N95 mask."
When can I come home?
That's the big question, of course. The CDC's 10-day guideline is what infectious disease doctors recommend as well. It's definitely prudent.
"We have isolation protocols for a reason – to reduce the spread for others," says Keri Althoff , an epidemiologist at the Johns Hopkins Bloomberg School of Public Health. And there is a risk of spread "if you're sitting next to someone on a plane" – or any kind of transportation, like a bus or train, that puts you near others. What's more, the person in the next seat could have underlying conditions that puts them at severe risk if they contract COVID.
But no authorities in the U.S. enforce the 10-day rule.
And waiting 10 days to end isolation can be a challenge.
"Being far away from home is not ideal. Home is more comfortable," says Dr. Preeti Malani , an infectious disease physician at the University of Michigan. Being stuck a few hundred miles or more from home when you're down with COVID can be stressful – you may feel pressured to return to work after 5 days off, face child care issues, worry about home and garden upkeep or whether your pet sitter can keep on the job.
"Don't underestimate the mental gymnastics of trying to figure out when to head home," says Althoff. "It's emotional, it's mental, it's financial. It's hard." And you're trying to make these decisions at a time when you're not feeling well.
What's more, even CDC advice is a bit confusing because there's another piece of its guidance that recommends 5 days of isolation after an infection while you're at home and not on a trip. For folks who aren't traveling, CDC says: "People with COVID-19 should isolate for 5 days and if they are asymptomatic or their symptoms are resolving (without fever for 24 hours), follow that by 5 days of wearing a mask when around others to minimize the risk of infecting people they encounter."
The end result is that many people are making their own decisions about when to travel.
Some travelers who just tested positive for COVID might say, I'm going home right now. BAD IDEA. Not only because they're putting others at risk, but because they may find that if the flight is long, they could grow sicker and sicker as the hours pass. All the experts who we interviewed agree: Don't do it!
(As an aside, our panel of experts also stressed that an uninfected traveler should assume that if they're on a plane, bus or train, there's going to be at least one passenger with COVID, which is a good reason to continue to mask up while traveling.)
Other COVID travelers might feel up to driving after, say, a few days, so they'd cancel the flight and rent a car – contact-free, of course – and head home. But, of course, that's easier to do if it's an 8-hour drive versus a 3-day expedition that involves finding places to stay and eat without putting others at risk.
And then there are folks who figure, maybe it's OK to isolate until they're feeling better – then they'll make the journey home. And maybe that's sooner than 10 days.
Keep in mind that you are typically most contagious in the 2 days prior to a positive test and the 5 days after, says Weatherhead.
"If you're feeling better and symptoms are going away after that 5-day period [when you're most infectious], travel is still not recommended — but putting on an N95 while traveling would be best," she says.
But symptoms aren't always a reliable barometer of your condition. "It's hard to know how infectious you are," she adds. Coughing of course is a way to spread the disease, but "a lot of people have coughs for weeks and that doesn't mean you are infectious."
Are tests useful?
The infected traveler might figure that a negative COVID test is a thumbs up to fly home. But you could test positive for many days after symptoms are gone – one NPR colleague saw the positive line pop up for 20 days. And the doctors we interviewed said by that time, you're likely not carrying enough viral load to infect others. Even if you are testing positive after, say, a week, "there is a very low probability of transmission if you are feeling asymptomatic," says Althoff.
So let's say your symptoms are pretty much gone — and it's been, oh, 5 to 7 days since you first tested positive. How do you travel without putting others at a big risk?
"If you feel bad, don't travel," says Baker.
But if you're feeling OK enough to make the journey, wear a mask – preferably an N95 that fits well. "In the name of goodness, think about those who are around you," says Baker.
Should you share your diagnosis with your seat mate?
A colleague had an interesting question. If you're flying home, say, a week after your first tested positive, should you inform an unmasked passenger next to you?
"I think that would cause pandemonium on the plane," says Baker. "I would keep my mask on and lean away." And maybe have a snack and a beverage in an isolated corner of the airport before you board the plane so you don't need to drop your mask for a bite or a sip.
Also, even though we're all pandemic weary, it's important to take stock of how far we've come. Here's Malani's assessment: "If two years ago you told me we'd have tests we can put in our pocket — and if we get sick, [be able to] call up a virtual portal and five minutes later get an antiviral prescription ... no one could have imagined that!"
Your Turn: Did you get COVID on a trip? How did you handle it?
Email [email protected] with the subject line "COVID on Vacation" and share your story. Include your full name and location, and we may include your response in a story on NPR.org. We are taking submissions until Tuesday, July 12. Update: This callout is now closed. Read some of our reader submissions here .
- coronavirus faqs
- coronavirus FAQ
An official website of the United States government
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
COVID-19 international travel advisories
Visitors to the U.S. do not need to be tested or vaccinated for COVID-19. U.S. citizens going abroad, check Department of State travel advisories for the country you will visit.
COVID-19 testing and vaccine rules for entering the U.S.
You do not need to show proof of being fully vaccinated against COVID-19 or take a COVID-19 test to enter the U.S. This applies to U.S. citizens and non-citizens.
U.S. citizens traveling to a country outside the U.S.
Find country-specific travel advisories, including COVID-19 restrictions, from the Department of State.
See the CDC's COVID-19 guidance for safer international travel to learn:
- If you can travel if you recently had COVID-19
- What you can do to help prevent COVID-19
LAST UPDATED: May 31, 2024
Have a question?
Ask a real person any government-related question for free. They will get you the answer or let you know where to find it.
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.

Heat Illnesses
Your chances of getting heat stroke, heat exhaustion, or other heat-related illness during travel depend on your destination, activities, level of hydration, and age. Learn ways to prevent, recognize, and treat heat-related illness .

Find a Clinic
Advice for Travelers
Personalized Health Information Tool for Global Travel
Frequently Asked Questions
CDC Yellow Book
Pre-travel Rapid Evaluation Portal for Patients
Clinician Resources
Research and Surveillance
- Medical Tourism
- Cholera Information for Health Care Professionals
- COVID-19 Travel Information
- Travel Industry Resources

Learn about CDC’s Traveler Genomic Surveillance Program that detects new COVID-19 variants entering the country.

Sign up to get travel notices, clinical updates, & healthy travel tips.
See the full list of Travel Health Notices , including:
Level 2 - Practice Enhanced Precautions
- New Zika in the state of Maharashtra, India August 22, 2024
- Updated Global Polio August 20, 2024
- New Oropouche in Cuba August 16, 2024
Level 1 - Practice Usual Precautions
- Updated Oropouche in South America August 16, 2024
- Updated Global Dengue August 14, 2024
- Updated Global Measles August 14, 2024
There are no Warning , Alert, Watch, COVID-19 Very High, COVID-19 High, COVID-19 Moderate, COVID-19 Low, COVID-19 Unknown, Level 4, or Level 3 notices currently in effect.
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Advertisement
Supported by
Omicron and Holiday Travel: 12 of the Most Pressing Questions
Vaccination requirements, testing rules, the new coronavirus variant and more: We answer your questions about traveling safely this holiday season.
- Share full article

By Julie Weed
Holiday travel suddenly feels more fraught as the world waits for emerging information on the transmissibility and virulence of the new coronavirus variant. Scientists are racing to see if the current vaccines offer protection against Omicron, but many families and other travelers may need to consider a variety of factors now before embarking to see relatives or to experience a change of scenery.
“Once again they will have to make informed decisions,” said Kathy Risse, a pediatrician in Seattle. But unlike last year’s holiday period, Dr. Risse said, “we know so much more about stopping transmission, and widespread testing is up and running.”
For those planning to travel, the basics for protection — vaccinations, masks and social distancing — will help make the trip safer. Here are answers to 12 of the most pressing travel questions for now.
What are the travel rules between U.S. states?
Currently there are no vaccine, testing or quarantine requirements to travel within the 50 United States, whether you fly, drive or go by rail — except Hawaii. Hawaii requires a 10-day quarantine for domestic travelers if they do not show proof of a full vaccination against the coronavirus or negative results from a test taken no more than 72 hours before their flight’s arrival.
Masks are still required by the Transportation Security Administration for passengers age 2 and up on planes, trains and buses . Different states, and even cities within states, may have their own mask, testing or vaccine requirements for activities such as indoor dining. Local health department sites or the AARP website are good starting places to research a state’s coronavirus rules.
Do you have to be vaccinated to fly domestically?
Again no, but C.D.C. guidelines recommend people delay travel until they are fully vaccinated .
Can we still go abroad?
Current C.D.C. guidance does not recommend international travel if you are not vaccinated. If you choose to travel overseas, it can be complicated: Your desired destination may have rules and guidelines that differ from those of the United States. Take Mexico , one of the most popular destinations for U.S. travelers. The country does not require vaccinations or testing for entry, regardless of the traveler’s nationality, while other countries, like Japan, Israel and Morocco , have recently closed their borders to noncitizens. To visit Canada , foreign visitors must show proof of vaccination and the negative results of a PCR or nucleic acid test. (Unvaccinated children can accompany vaccinated adults into Canada but must follow a specific set of protocols including health questionnaires and a virus test.)
Rules for these and other countries can change at any time, so it’s best to keep checking official government websites as your travel date approaches. The Times updates a list of countries open to U.S. citizens and the C.D.C. maintains a list of global Covid hot spots .
Do you have to be vaccinated to fly internationally?
Again, it’s complicated. For outbound travel from the United States, vaccination requirements depend on your destination. U.S. embassy sites are good sources of information, as are countries’ tourist and health sites for your desired destination. Age requirements can also vary by destination.
U.S. citizens do not have to be vaccinated to travel back to the United States, but most adult foreign travelers do. Exceptions can be found on the C.D.C. website. Children under 18 are exempted from the vaccination requirement.
What are the testing requirements for adults and children flying into the United States?
The United States recently changed the timing of its testing requirement to re-enter the country. Travelers must now submit a negative virus test result taken within one day of the flight’s departure, instead of the previous three-day requirement for vaccinated fliers. This applies to all travelers age 2 and up, regardless of nationality or vaccination status.
It is important to note that the requirement is “one day” rather than “24 hours.” For example, for a flight leaving on Sunday at 3 p.m., the test needs to be taken anytime on Saturday or anytime on Sunday. This gives fliers more flexibility in scheduling their test for any time the day before the flight, or the day of, rather than timing a nighttime test for a flight the next evening.
Should we bring some at-home test kits with us?
Not a bad idea. The Food and Drug Administration has approved 13 home-based Covid tests , and families may want to bring some on the trip to use if anyone comes down with the sniffles or a cough, or to take just before getting to Grandma’s. They may be hard to find in stores or limited to one or two per customer, so don’t leave this errand to the last minute.
Family members may have varying risk tolerances, and at-home tests can help people relax and enjoy each other’s company, Dr. Risse said, “because even though it is imperfect, it adds another layer of protection.”
The C.D.C. specifies which tests are allowed for entry into the United States. Self-tests for the virus are OK if there is an accompanying telehealth service providing “real-time supervision remotely through an audio and video connection.” Your hotel or local family members may be able to point you to other testing options in the country — like at medical clinics or pharmacies.
What are the vaccine rules on cruise ships?
Rules vary by cruise line. On Disney cruises , passengers 12 and up must be vaccinated, but that age is moving to 5 beginning Jan. 13. Children under 5 must have a negative virus test taken within three days of departure. Princess Cruise Line and Norwegian Cruise Line are only welcoming vaccinated travelers ages 5 and up. Currently, children under 5 are not allowed on board. Royal Caribbean requires guests age 12 and up to be vaccinated.
There may be additional requirements for cruises docking at other countries. Travelers boarding a cruise in Barbados, for example, need to download the BIMsafe app and follow its directions. It’s best to check with each cruise line for a specific sailing’s current rules and protocols.
Cruise lines have reason to worry, as “their whole image as a sector hangs in the balance,” said Lynn Minnaert, a clinical associate professor at the Jonathan M. Tisch Center of Hospitality at New York University . “They are taking vaccinations and testing seriously, so passengers who bear in mind the risks and take common sense precautions should have a safe experience.”
The C.D.C. still recommends that people who are unvaccinated or at risk of severe illness (regardless of vaccination status) avoid traveling on cruise ships worldwide, including river cruises.
Can we go to theme parks?
Theme parks are required to follow state rules. Disneyland in California and Disney World in Florida require guests 2 and older to wear masks in indoor locations, lines and enclosed transportation except when actively eating or drinking. Universal Studios in Florida recommends masking indoors but has no coronavirus-focused guest requirements.
Is my child fully protected if they have had two vaccine doses?
Fully vaccinated, as defined by the C.D.C. as two weeks after the second dose , is not the same as fully protected. Breakthrough cases occur but they are generally mild. Scientists are still examining incoming data to determine if the vaccines will protect against the Omicron variant. In the meantime, the advice from the C.D.C. still stands: children 5 and older should get the vaccine to protect them and those around them from getting Covid-19 disease.
How can I help my child wear their mask while traveling?
Keeping a mask on a young child while traveling can be challenging for children and parents. Here are some ideas to help your child comply with the rule: Practice wearing a mask together days or weeks before the flight so they get used to the feel. Go slow and don’t make it a fight. Try out different masks for comfort and fit. You may bring different ones to “change into” to make things fun or have a matching mask for a stuffed animal. If your child gets agitated on the flight stay as calm as you can because they will take their emotional cues from you. And consider resorting to bribery — more screen time, or bring small wrapped gifts they can open each time they have kept the mask on for some period of time.
Should we hunker down between when we get our tests and when we travel?
It couldn’t hurt, especially if you are traveling to see older or immune-compromised relatives, no matter their vaccination status.
Should we still go?
“Families come to me asking for a ‘Yes’ or ‘No’ answer on if they should travel, because they are so tired of making the day-to-day risk assessments,” said Dr. Risse, the pediatrician. But every family needs to make its own decision to travel, based on the importance of their trip, how protected family members are and how much they trust fellow travelers to abide by the masking and social distancing rules that keep people safer. They also need to be aware of the levels of cases at their destination and the level of exposure their potential activities present. That is, eating at a restaurant indoors or staying at a hotel instead of a private residence.
Vivek Garg , chief medical officer for the health insurer Humana’s senior-focused primary care business, encourages travel when C.D.C. guidelines are followed. “It’s important for everyone’s mental health, especially that of older adults, that we socialize with friends and family,” Dr. Garg said.

52 Places to Love in 2021
We asked readers to tell us about the spots that have delighted, inspired and comforted them in a dark year. Here, 52 of the more than 2,000 suggestions we received, to remind us that the world still awaits.
Follow New York Times Travel on Instagram , Twitter and Facebook . And sign up for our weekly Travel Dispatch newsletter to receive expert tips on traveling smarter and inspiration for your next vacation.
An earlier version of this story omitted that one U.S. state, Hawaii, has entry requirements for domestic travelers. American travelers wishing to enter Hawaii must show proof of vaccination, a negative test result or they must quarantine for 10 days. There are no vaccine, testing or quarantine requirements for domestic travel to the other 49 states.
How we handle corrections
An official website of the United States government Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

Plan your Travel
⚠ The COVID-19 Public Health Emergency expired as of May 11, 2023. This site will no longer be updated and will remain online for historical purposes only.
For current COVID-19 guidance, please visit the Centers for Disease Control and Prevention (CDC) .

- Before booking your trip, check for international travel advisories and destination-specific COVID-19 risk . Refer to individual state, territorial, tribal, and local government websites for domestic travel advisories and information about quarantine or other restrictions.
- The UNWTO-IATA Destination Tracker is a free online tool for travelers to get information on COVID-19 requirements for international travel and the measures in place at the destination.
- Review CDC’s considerations for Travel During COVID-19 before you go to determine your personal risk.
- Pack Smart! Pack Safe! Know what is in your carry-on and checked bags and make sure there are no prohibited items inside before arriving at the checkpoint. As a temporary exemption from the 3-1-1 rule, TSA is allowing one oversized liquid hand sanitizer container, up to 12 ounces per passenger, in carry-on bags. These will need to be placed in a bin during the screening process. Passengers may also bring hand wipes through checkpoints.
- Unused COVID-19 test kits do not contain dangerous goods and are typically allowed in both carry-on and checked baggage.
- COVID-19 test kits containing diagnostic samples (e.g., nasal swabs and vials of sputum) are not allowed in carry-on baggage. These samples must be properly packaged, handled, and identified as a UN3373 Category B Infectious Substance (PDF) during transportation. Passengers should check with their carrier before packing COVID-19 test kits containing diagnostic samples in checked baggage or shipping as cargo. Individual carriers and international requirements may be more restrictive than domestic regulations. Visit FAA’s Pack Safe site for more information.
- CDC recommends wearing a mask throughout your travel experience.
- Consider joining TSA PreCheck ™. Members continue to be eligible for expedited screening procedures and have the shortest wait times. TSA PreCheck provides the most convenience and least amount of physical contact at the TSA checkpoint. Visit TSA PreCheck to enroll today.
- Have a travel plan that does not rely on the U.S. government for assistance. Visit travel.state.gov for more information.
- Make two copies of all your travel documents in case of emergency, and leave one with a trusted friend or relative.
- Remember, if you are sick, stay home and do not travel! Contact your airline regarding their re-booking and cancellation policies .
*All information developed in accordance with CDC guidelines.
- Credit cards
- View all credit cards
- Banking guide
- Loans guide
- Insurance guide
- Personal finance
- View all personal finance
- Small business
- Small business guide
- View all taxes
You’re our first priority. Every time.
We believe everyone should be able to make financial decisions with confidence. And while our site doesn’t feature every company or financial product available on the market, we’re proud that the guidance we offer, the information we provide and the tools we create are objective, independent, straightforward — and free.
So how do we make money? Our partners compensate us. This may influence which products we review and write about (and where those products appear on the site), but it in no way affects our recommendations or advice, which are grounded in thousands of hours of research. Our partners cannot pay us to guarantee favorable reviews of their products or services. Here is a list of our partners .
Why Don’t We Know If People Are Getting COVID on Planes?

Many, or all, of the products featured on this page are from our advertising partners who compensate us when you take certain actions on our website or click to take an action on their website. However, this does not influence our evaluations. Our opinions are our own. Here is a list of our partners and here's how we make money .
It seems like all my friends got COVID this summer, and many think they got it on a plane. But that’s as anecdotal as data gets. What does, you know, science have to say?
I talked to Arnold Barnett, a professor of statistics at the Massachusetts Institute of Technology, who co-wrote a recent paper that modeled the risk of contracting COVID while flying early in the pandemic. He and his student combed through the available data and built a complex mathematical model to determine the risk of getting infected onboard. Yet they ran into limitations, because no organized effort was made by the U.S. or any country to systematically contact trace COVID transmissions onboard aircraft.
“Nobody is screened. Nobody is asked if they’ve come down with COVID,” he explains. “There was no attempt made to figure out where people got it. We have so little data.”
That’s right, of all the billions spent combating the virus, supplying at-home testing kits and bailing out the airlines , little to none of it was spent answering the basic question of where and how people actually contracted the disease in the first place. Models like Barnett’s, while helpful, offer only best guesses.
“If we had actual data from the United States, then maybe we wouldn’t have needed a model,” he says.
One systematic attempt to contact trace on a flight that landed in Vietnam found that, of the 16 passengers who tested positive, 12 were in business class, where the one symptomatic case was found. In other words, a bunch of high-price ticket holders at the front of the plane got sick from the same person.
Yet this study from Vietnam's National Institute of Hygiene and Epidemiology was performed in March 2020. Think of what could have happened if we had kept collecting data throughout the pandemic.
Unknown unknowns
Cast your mind back to fall 2020. The first COVID wave had passed and would-be travelers were wondering: Is it safe to fly home for the holidays ?
The Centers for Disease Control and Prevention, based on a bizarre study commissioned by many federal agencies involving mannequins coughing at one another, suggested that “most viruses and other germs do not spread easily on flights because of how air circulates and is filtered on airplanes.”
You may remember that study. You may not know (as I didn’t, until recently) that the researchers who performed it received so much criticism that they appended a disclaimer, suggesting the study’s findings “were not designed to provide actionable information about viral risk during flight, safe flight times or seating capacity.”
The CDC has removed its messaging and references to the study, while airlines such as United Airlines continue to cite it as evidence of air travel safety.
The United Airlines website still mentions the problematic study.
I was writing about all this in 2020, trying to parse these confusing messages, and I used the mannequin study as evidence that flying wasn’t as dangerous as we originally thought.
Turns out I was wrong, but never even learned I was wrong until years later.
The real problem isn’t one poorly interpreted study. It’s that we still don’t know the rate at which people contracted (and died from) COVID after getting on a plane. Were 1% of COVID cases caused by air travel? Or 10%? More?
We have no idea, and that could have major ramifications down the road.
Flying into the unknown
Barnett’s model spit out a nice round number, suggesting the odds of contracting COVID on a full two-hour flight were about 1 in 1,000 at the beginning of the pandemic. But he believes the risks have probably increased significantly since then.
“Omicron BA.5 is a lot more contagious than the earlier versions," Barnett says. "And now people by and large are not wearing masks on airplanes.”
Thankfully, vaccines and treatments have reduced the mortality rate of COVID, so the risks are more manageable. But what if a new variant emerges that — knock on wood — evades vaccines altogether? Or (no, really, knock on wood) causes serious illness in young people or children? We will all want a real answer to simple questions: How bad is COVID transmission on planes? Is any one airline safer than another ?
Maddeningly, bafflingly, head-scratchingly, we still don’t know for sure.
“All models are wrong, some are useful,” Barnett says with a wry grin.

on Chase's website
1x-5x 5x on travel purchased through Chase Travel℠, 3x on dining, select streaming services and online groceries, 2x on all other travel purchases, 1x on all other purchases.
60,000 Earn 60,000 bonus points after you spend $4,000 on purchases in the first 3 months from account opening. That's $750 when you redeem through Chase Travel℠.

1.5%-5% Enjoy 5% cash back on travel purchased through Chase Travel℠, 3% cash back on drugstore purchases and dining at restaurants, including takeout and eligible delivery service, and unlimited 1.5% cash back on all other purchases.
Up to $300 Earn an additional 1.5% cash back on everything you buy (on up to $20,000 spent in the first year) - worth up to $300 cash back!

on Capital One's website
2x-5x Earn unlimited 2X miles on every purchase, every day. Earn 5X miles on hotels, vacation rentals and rental cars booked through Capital One Travel, where you'll get Capital One's best prices on thousands of trip options
75,000 Enjoy $250 to use on Capital One Travel in your first cardholder year, plus earn 75,000 bonus miles once you spend $4,000 on purchases within the first 3 months from account opening - that’s equal to $1,000 in travel.

A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- NCIRD Divisions and Offices
- About NCIRD
- Investigations
- NCIRD PRESS
- Career Opportunities
- Contact NCIRD
- View All Home
CDC's Updated Respiratory Virus Guidance: What to Do When You Are Sick
CDC released updated Respiratory Virus Guidance in response to the decreasing risk that COVID-19 poses to the population. This updated Guidance includes strategies to protect people at highest risk of getting seriously ill and provides actionable recommendations for people with common viral respiratory illnesses, including COVID-19, flu, and RSV.

What CDC knows
As the 2023-2024 fall and winter virus season ends, it’s clear that the situation surrounding COVID-19 has changed. It is still an important health threat, but it is no longer the emergency that it once was, and its health impacts increasingly resemble those of other respiratory viral illnesses, including flu and RSV.
What CDC is doing
What is the updated guidance?
Protect yourself from getting sick:.
The most important thing you can do to protect yourself from COVID-19, flu, and RSV is to stay up to date on your recommended vaccines. Even when vaccines don't prevent infection, they often tame these viruses, reducing severity, and preventing their worst outcomes, like hospitalization and death.
Along with staying up-to-date on your vaccines, practicing good hygiene by covering your coughs and sneezes, washing or sanitizing your hands often, and cleaning frequently touched surfaces can help. Also, taking steps for cleaner air can help reduce the spread of respiratory viruses. This can mean bringing in fresh outside air by opening a window, purifying indoor air, or having outdoor social activities.
If You Get Sick:
Even if you practice these core prevention strategies, you may still catch a virus and develop respiratory symptoms. If that happens, the updated Guidance recommends two actions:
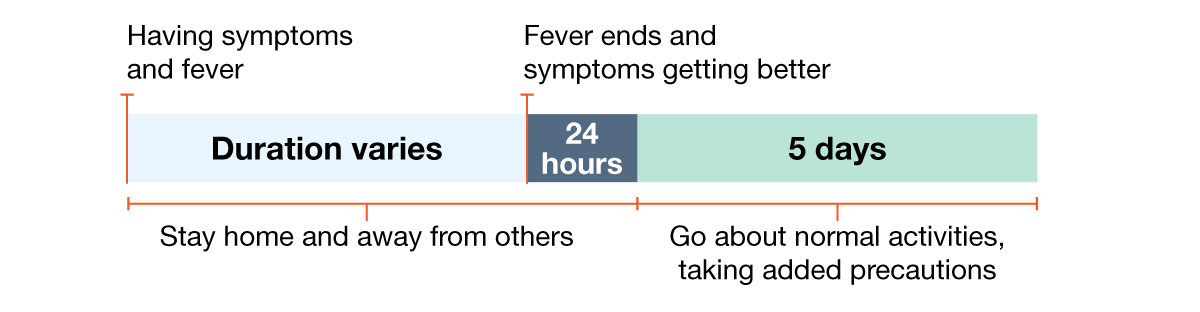
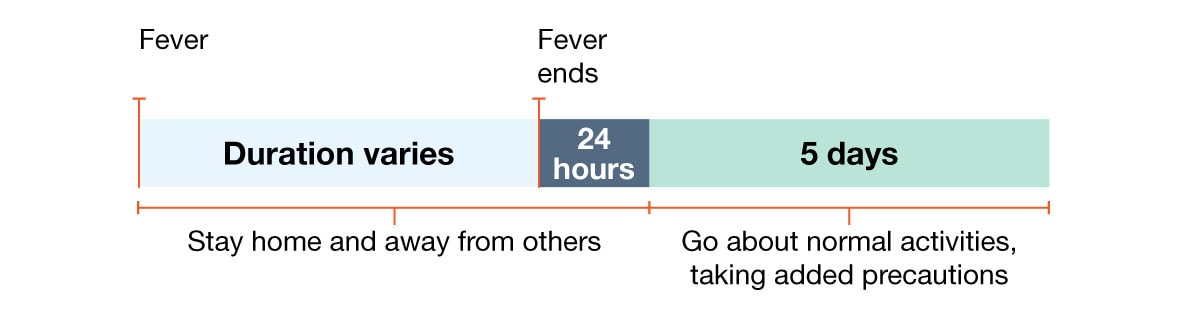
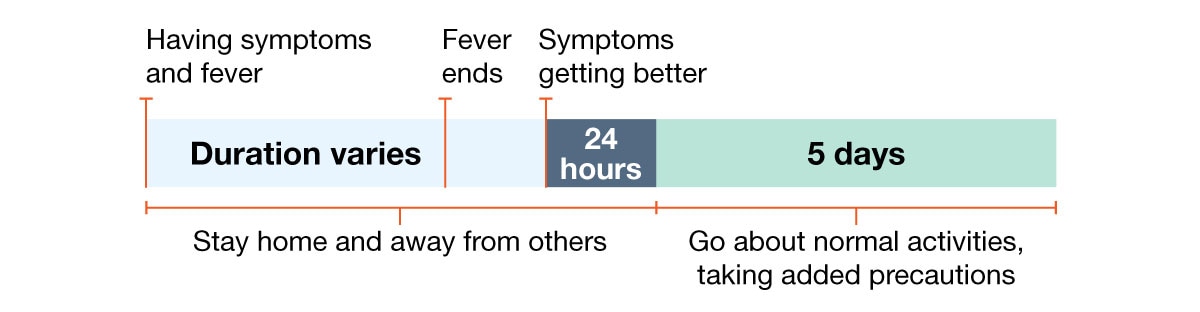
Step 1: Stay at home.
As much as possible, you should stay home and away from others until at least 24 hours after both:
- Your symptoms are getting better overall, and
- You have not had a fever (and are not using fever-reducing medication).
This advice is similar to what has been recommended for flu for decades and will help reduce the spread of COVID-19 and other respiratory viruses during the most contagious period after infection. Not all respiratory virus infections result in a fever, so paying attention to other symptoms (cough, muscle aches, etc.) is important as you determine when you are well enough to leave home.
If your symptoms are getting better, and stay better for 24 hours, you are less likely to pass your infection to others and you can start getting back to your daily routine and move on to step 2.
Step 2: Resume normal activities and use added prevention strategies over the next five days.
This may include taking more steps for cleaner air, enhancing your hygiene practices, wearing a well-fitting mask, keeping a distance from others, and/or getting tested for respiratory viruses. People can choose to use these prevention strategies at any time. Since some people remain contagious beyond the "stay-at-home" period, taking added precautions can lower the chance of spreading respiratory viruses to others.
People who are at higher risk for severe illness who start to feel sick should seek health care right away so that they can access testing and/or treatment. Early treatment for COVID-19 or flu may prevent severe disease in people at higher risk, even if they are up to date with their vaccines.
Depending on your circumstances, here are a few examples of what updated guidance could look like if you come down with a respiratory infection:
Example 1: Person with fever and symptoms.
Example 2: Person with fever but no other symptoms.
Example 3: Person with fever and other symptoms, fever ends but other symptoms take longer to improve.
Example 4: Person gets better and then gets a fever.

Why was the guidance updated?
We are in a different place with covid-19 than we were..
Weekly hospital admissions for COVID-19 have decreased by more than 75% and deaths by more than 90% compared to January 2022. Importantly, these decreases have continued through a full respiratory virus season, despite levels of viral activity similar to prior years.
Almost 98% of people in the United States have antibodies against COVID-19 because of prior vaccination, infection or both. We also have effective and widely available vaccines and treatment that work, but more than 95% of people hospitalized with COVID-19 this last season were not up to date on COVID-19 vaccines and most had not received antiviral treatment.
The updated guidance change will not significantly increase COVID-19 community spread and severe disease.
Real-world experience in states like Oregon and California and countries like the UK, Australia, Denmark, France, Norway, and Canada found no significant change in spread or severe disease after implementing similar guidance updates.
Clear, simple, and actionable guidance, regardless of the respiratory virus, will help protect Americans.
Symptoms are an easy way to know when someone should use prevention strategies. These strategies, like staying home, can be done without a test. A CDC survey found that a majority of Americans take precautions when sick with cold or cough symptoms (such as avoiding contact with people at higher risk and avoiding large indoor gatherings) even if they don't know what virus is causing the illness. Different guidance for different viruses makes it difficult to make a prevention plan when you don't know what is causing your symptoms.
Keeping you healthy: CDC's work continues
COVID-19, flu, and RSV contribute to severe illness and disruptions in our everyday lives. CDC remains committed to protecting everyone's health, and will continue to provide information about respiratory virus activity to inform people on what actions they can take to stay healthy. This includes informing people with a range of risk factors that can increase the chance of getting very sick (severe illness). Generally, people at higher risk of severe illness from respiratory viruses are older adults, young children, people with compromised immune systems, people with disabilities, and pregnant people. CDC has included additional guidance for these populations to help protect them from severe illness.
Information on NCIRD's mission, work, and organizational structure.
- Biochemistry and Molecular Biology
- Biostatistics
- Environmental Health and Engineering
- Epidemiology
- Health Policy and Management
- Health, Behavior and Society
- International Health
- Mental Health
- Molecular Microbiology and Immunology
- Population, Family and Reproductive Health
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
What to Know About the Updated COVID Vaccine for Fall, Winter 2024–25
The updated COVID vaccine provides safe, effective protection against current variants for everyone 6 months and older.
Aliza Rosen
Editor’s note: This article was updated on September 3, 2024 to include information on the updated Novavax COVID-19 vaccine, which was authorized by the FDA on August 30, 2024.
Amid an unexpectedly large surge of summer COVID infections in the U.S., and with the fall/winter virus season around the corner, updated COVID vaccines have arrived.
COVID vaccines are one of the best and safest ways to protect against severe illness and hospitalization. Updated COVID vaccines, also referred to as boosters, are chosen to target the variants currently circulating and are recommended for everyone 6 months of age and older.
In this Q&A, Andy Pekosz , PhD, a professor in Molecular Microbiology and Immunology , discusses who the updated vaccine is recommended for, when to get yours, whether it’s safe to get it alongside other seasonal vaccines.
What’s new about this year’s updated COVID vaccines?
As in previous years, there are mRNA vaccines—one from Moderna, one from Pfizer—and a protein-based vaccine, from Novavax. One nuance this year is that the mRNA and protein-based vaccines target different—though closely related—variants.
The updated mRNA COVID vaccines from Moderna and Pfizer are based on the KP.2 strain, one of the FLiRT variants that have been spreading since early spring. These variants and their sub-variants have caused the majority of infections during this summer’s COVID wave. The protein-based Novavax vaccine is based on the JN.1 variant, which accounted for the majority of COVID infections in the first few months of 2024 and is the parent strain from which KP.2 and other currently circulating variants branch from.
At the end of the day, laboratory experiments show that all of the updated vaccines available this season can recognize circulating COVID variants and therefore should be similarly effective in reducing your chance of becoming severely ill from COVID infection or needing to be hospitalized.
Who should be getting an updated COVID vaccine?
Everyone 6 months and older should get vaccinated against COVID, according to the CDC’s recommendations .
For children ages 6 months to 4 years: Vaccination is recommended, but the number of vaccinations is based on which vaccine they receive, their age, and whether they’ve received a previous COVID vaccine. Parents and guardians should refer to CDC guidance and check with their pediatrician to see what’s recommended for their child.
For people ages 5 years and up: One dose of the updated COVID vaccine is recommended, regardless of whether they’ve been vaccinated previously. If someone has received a COVID vaccine recently, they should wait at least two months before getting the updated one for this season.
According to updated CDC guidelines, individuals who are immunocompromised may receive additional doses with their health care provider’s guidance.
When is the best time to get vaccinated?
This summer’s surge has been larger and lasted longer than many experts anticipated, making it a little trickier than years past to determine the best time to get vaccinated.
People who have not had COVID in the past few months have a couple options:
- Get the updated COVID vaccine as soon as it’s available (late August, early September) to protect yourself as the wave of summer infections continues.
- Get the updated COVID vaccine around mid-October to boost protection in time for the rise of cases that typically occur around November through January.
People at higher risk of severe illness should consider getting an updated COVID vaccine as soon as possible. Everyone who is eligible should get an updated COVID vaccine by mid-October in order to build immunity ahead of holiday travel and gatherings. Remember, it takes about two weeks to build up immunity following a vaccine, so schedule your vaccination accordingly.
How long does protection last after I'm vaccinated?
Broadly speaking, the COVID vaccine provides strong protection against infection for up to three months and protection against severe disease out to six months. That said, there are a lot of variables that can affect duration and strength of protection, including any new variants that may emerge and how different they are from the vaccine formulation.
If I had COVID recently, when should I get the updated vaccine?
If you’ve had COVID this summer, you’ll have strong infection-based immunity and can wait a few months after your infection before getting the vaccine. According to the CDC, you can wait three months since your symptoms began or, for asymptomatic cases, since you first tested positive.
There’s some evidence to support waiting as long as six months after a COVID infection to receive an updated vaccine. Waiting longer than the CDC’s guidance of three months is not recommended for high-risk groups, but it’s something people can discuss with their doctor.
How should I choose which COVID vaccine to get?
Between the two mRNA vaccines from Moderna and Pfizer, there is no reason to get one over the other. They target the same KP.2 variant, are similarly effective, and elicit similar side effects.
The same goes for deciding between the mRNA vaccines and the Novavax protein-based vaccine: While they target different variants, they both will recognize current variants. People who have had a particularly adverse response to a previous mRNA vaccine might consider the Novavax vaccine as an alternative, as protein-based vaccines generally don’t induce as strong side effects.
Is the COVID vaccine free?
The COVID vaccine is free under most health insurance plans and Medicare.
If you don’t have insurance to cover the cost of the COVID vaccine, look for vaccination clinics run by your local or state health department. Children under 18 may also be eligible to get a free COVID vaccine through the CDC’s Vaccines for Children Program .
You can find local pharmacies offering COVID vaccines at Vaccines.gov or by contacting your health care provider or local health department .
Are there any side effects to the updated COVID vaccine?
The common side effects are the same as with previous COVID vaccines. Symptoms like soreness at the injection site, achiness or joint pain, fatigue, slight fever, chills, or nausea are normal and not cause for concern. These side effects are a sign that your body is mounting an immune response—exactly what it’s supposed to do following a vaccine. Side effects generally subside within a day or two.
If I haven’t gotten any COVID vaccines yet, can I start with this one?
If you’ve never been vaccinated against COVID, now is a great time to start. People 5 years of age and older are considered up to date on COVID vaccination once they receive one dose of an updated mRNA COVID vaccine.
People 12 years and older who have not previously received a COVID vaccine and choose the Novavax vaccine are considered up to date after receiving two doses of the Novavax vaccine, with the second dose administered three weeks after the first one.
How well does the vaccine protect against the variants currently circulating?
The vaccine is a close match to variants currently circulating and provides good protection against severe disease, hospitalization, and death. While KP.2 is not causing a significant number of infections, the most prevalent variants circulating right now are very closely related to them. The vaccine will never be a perfect match to the circulating variants because it takes 2-4 months to make the vaccine, and during that time the virus continues to change as it infects people.
Is vaccine-induced immunity better than immunity from infection?
Vaccine-induced immunity is better because it’s safer. When you get infected with COVID, symptoms from the infection wreak havoc on your body. Whether or not you’ve been infected or vaccinated previously, the COVID booster is going to strengthen your immune responses to high levels and do so in a safe way.
Can I still get COVID if I’m vaccinated?
People who are vaccinated can still get COVID, but it is much more likely they will experience mild symptoms. Vaccinated people are much less likely to experience severe illness or get so sick that they need to be hospitalized. Data continue to show that those who are hospitalized with COVID are largely people who have not received a COVID vaccine within the past 12 months.
Particularly for people at higher risk of severe COVID, vaccination is an essential tool for reducing COVID complications, hospitalization, and death.
Can you get the flu shot and the COVID vaccine at the same time?
Yes! In fact, studies have shown that people who decide to spread out their vaccines into separate appointments often don’t follow through with getting both. We’ve also seen that the immune response generated by each vaccine does not change based on whether they are administered at the same time or separately.
It’s important to remember that many of the same populations at high risk of experiencing severe illness from COVID are also at high risk of severe influenza. Especially for these vulnerable populations, it’s a good idea to time your vaccines together.
When might we see a combined COVID and flu vaccine?
Some vaccine manufacturers have been working on developing a combined vaccine for COVID and flu, but we’re not there yet. We certainly won’t see a combined vaccine this year. It’s possible one will be ready in time for fall 2025, but we won’t know for sure until more clinical trial results are available.
Aliza Rosen is a digital content strategist in the Office of External Affairs at the Johns Hopkins Bloomberg School of Public Health.
Related Articles:
- Understanding the CDC’s Updated COVID Isolation Guidance
- What to Know About COVID FLiRT Variants
- The Long History of mRNA Vaccines
Related Content
A ‘Critical Pathogen’: The Rise of Drug-Resistant Fungal Diseases

Why We’re Still Waiting for a Pandemic Treaty

Why COVID Surges in the Summer

The Visible and Unseen Dangers Lurking in Floodwater

Public Health Prep for the 2024 Paris Olympics
- Travel Advisories |
- Contact Us |
- MyTravelGov |
Find U.S. Embassies & Consulates
Travel.state.gov, congressional liaison, special issuance agency, u.s. passports, international travel, intercountry adoption, international parental child abduction, records and authentications, popular links, travel advisories, mytravelgov, stay connected, legal resources, legal information, info for u.s. law enforcement, replace or certify documents.
Share this page:
Uganda Travel Advisory
Travel advisory december 28, 2023, uganda - level 3: reconsider travel.
Uganda Level 3 – Reconsider Travel C T O
Reissued with updates to terrorism information.
Reconsider travel to Uganda due to crime, terrorism , and anti-LGBTQI+ legislation . Some areas have increased risk. Read the entire Travel Advisory.
Country summary: There remains a threat of terrorist attacks in Uganda and throughout the region. Numerous terrorist attacks have occurred in Uganda, to include religious venues, schools, and areas frequented by tourists, resulting in the deaths of Ugandans as well as foreign visitors. U.S. citizens should remain alert and avoid large public gatherings. In October 2023, ISIS-Central Africa claimed responsibility for killing two international tourists and a Ugandan driver within Queen Elizabeth National Park.
Violent crime , such as armed robbery, home invasion, and sexual assault, presents a serious threat to those visiting and residing in Uganda and can occur at any time, especially in larger cities, including Kampala, Jinja and Entebbe, in the Karamoja region, and along Uganda’s western and northern borders. Local police may lack appropriate resources to respond effectively to serious crime in most areas.
The May 2023 Anti-Homosexuality Act raises the risk that LGBTQI+ persons, and those perceived to be LGBTQI+, could be prosecuted and subjected to life imprisonment or death based on provisions in the law , and may be subject to mandatory reporting to the police if they are suspected of committing or intending to commit acts in violation of the law, and could face harassment or attacks by vigilantes. Those perceived to support the dignity and human rights of LGBTQI+ persons (including those of youth under the age of 18) could be prosecuted and imprisoned for multi-year sentences. Even an unsubstantiated accusation of supporting the LGBTQI+ community can create risks from police and vigilantes. Read the country information page for additional information on travel to Uganda.
If you decide to travel to Uganda:
- Remain alert and avoid large public gatherings.
- Keep a low profile.
- Be aware of your surroundings.
- Do not display signs of wealth, such as expensive watches or jewelry.
- Use caution when walking or driving at night.
- Remain with a group of friends in public.
- Do not physically resist any robbery attempt.
- Do not open your door for people at your hotel/residence unless you know who it is.
- Do not leave food and drinks unattended in public, especially in local clubs.
- Stay alert in locations frequented by foreign tourists.
- Be extra vigilant when visiting banks or ATMs.
- Carry a copy of your passport and visa (if applicable) and secure originals in your hotel safe.
- Provide your itinerary to a family member or friend.
- Enroll in the Smart Traveler Enrollment Program (STEP) to receive Alerts and make it easier to locate you in an emergency.
- Be mindful that any public identification with the LGBTQI+ community, as either a member or supporter, could be grounds for prosecution, and that even private consensual same-sex relations are illegal.
- Follow the Department of State on Facebook and Twitter .
- Review the Country Security Report for Uganda.
- Prepare a contingency plan for emergency situations. Review the Traveler’s Checklist.
- Visit the CDC page for the latest Travel Health Information related to your travel.
Travel Advisory Levels
Assistance for u.s. citizens, search for travel advisories, external link.
You are about to leave travel.state.gov for an external website that is not maintained by the U.S. Department of State.
Links to external websites are provided as a convenience and should not be construed as an endorsement by the U.S. Department of State of the views or products contained therein. If you wish to remain on travel.state.gov, click the "cancel" message.
You are about to visit:

IMAGES
COMMENTS
THE O.A.T. COMMUNITY Harriets Corner The Inside Scoop ... The Leader in Solo Travel. Discover why more than 42,000 travelers are joining us solo through 2023. Learn More . ... Covid-19 Health & Safety: Land Adventures Covid 19-Health & Safety: Small Ships NEW O.A.T. Travelflix ...
Flight delays; missed connections; baggage delayed, lost, or damaged; a medical emergency—be prepared for unexpected events with our Travel Protection Plan. Trip Interruption: We protect up to 150% of Trip Cost (more than the price of your trip) in the event of a trip interruption, while other plans cover the base cost your trip.
Wear a mask on public transportation and in airports, stations, and other travel hubs. Keep your distance from people who aren't traveling with you. Wash your hands often or use a hand sanitizer ...
COVID-19 spread during travel. The virus that causes COVID-19 spreads mainly from person to person. When the virus is spreading, spending time indoors with a crowd of people raises your risk of catching it. The risk is higher if the indoor space has poor airflow. The coronavirus is carried by a person's breath.
All O.A.T. travelers must be fully vaccinated against COVID-19 at least 14 days prior to departure, and all Trip Experience Leaders, ship crew, and coach drivers will be vaccinated as well ...
Travel may increase your chance of getting and spreading COVID-19. Postponing travel and staying home is the best way to protect yourself and others from COVID-19. Delay travel if you are waiting for test results, test positive, are sick, or have been around someone with COVID-19 in the past 14 days. Find out more about When to Delay Travel.
What to Know About the C.D.C. Guidelines on Vaccinated Travel. In updated recommendations, the federal health agency said both domestic and international travel was low risk for fully vaccinated ...
It is important that you assess your risk of COVID-19 and follow these simple prevention measures throughout your travel: wear a well-fitting mask and keep a safe distance from others, as feasible. always practice respiratory etiquette by covering coughs and sneezes. stay home if you are sick and consider not travelling.
Interest in international air travel is rising. If you're want to fly out of or into the United States, there's a lot you need to know. Here are answers to key questions.
A group of 26 organizations sent a letter to White House COVID-19 czar Jeffrey Zients urging the federal government "to partner with us to develop, by May 1, 2021, a risk-based, data-driven ...
[Read our 2021 Travel questions and answers guide on restrictions, vaccination and more.]. If you want to find out if you currently have the coronavirus, you should plan on taking a virus test ...
Since October 2020, the WHO Guideline Development Group for International Travel and Health (WHO ITH GDG) is tasked with regularly evaluating the scientific evidence around the effectiveness, safety and impact of public health measures for reducing travel-associated spread of SARS-CoV-2, the virus that causes COVID-19, while avoiding unnecessary interference with international traffic.
The COVID experts we interviewed suggest these pre-trip steps: Pack self-tests and high quality (N95 or KN95) masks. Because you sure don't want to have to hunt them down in an unfamiliar place ...
U.S. citizens traveling to a country outside the U.S. Find country-specific travel advisories, including COVID-19 restrictions, from the Department of State. See the CDC's COVID-19 guidance for safer international travel to learn: If you can travel if you recently had COVID-19. What you can do to help prevent COVID-19. LAST UPDATED: May 31, 2024.
Highlights. Learn about CDC's Traveler Genomic Surveillance Program that detects new COVID-19 variants entering the country. Sign up to get travel notices, clinical updates, & healthy travel tips. CDC Travelers' Health Branch provides updated travel information, notices, and vaccine requirements to inform international travelers and provide ...
Just when we thought travel rules were stabilizing, along comes the Omicron variant of the coronavirus. Read this Q&A for the latest updates on new US travel rules.
But unlike last year's holiday period, Dr. Risse said, "we know so much more about stopping transmission, and widespread testing is up and running.". For those planning to travel, the basics ...
But in order to avoid riding in style with germs, there are some precautions you should take before you hit the road. Start by cleaning and disinfecting your vehicle thoroughly. Wipe down all high ...
A safe start to your travel begins at home. Before booking your trip, check for international travel advisories and destination-specific COVID-19 risk.Refer to individual state, territorial, tribal, and local government websites for domestic travel advisories and information about quarantine or other restrictions.; The UNWTO-IATA Destination Tracker is a free online tool for travelers to get ...
With all the energy devoted to air travel and COVID safety, you'd think we'd have some hard data. We don't. Updated Aug 12, 2024 7:21 a.m. PDT · 3 min read.
It's important to remember that COVID-19 is not a winter-only virus and can still spread during the summer. If you're taking a flight or any other public transportation, don't forget to pack masks and practice good hand hygiene. Masks protect you from COVID-19 and other respiratory viruses, and good hand hygiene habits can help prevent ...
COVID-19. COVID-19 (coronavirus disease 2019) is a disease caused by a virus named SARS-CoV-2. It can be very contagious and spreads quickly.
CDC released updated Respiratory Virus Guidance in response to the decreasing risk that COVID-19 poses to the population. This updated Guidance includes strategies to protect people at highest risk of getting seriously ill and provides actionable recommendations for people with common viral respiratory illnesses, including COVID-19, flu, and RSV.
Editor's note: This article was updated on September 3, 2024 to include information on the updated Novavax COVID-19 vaccine, which was authorized by the FDA on August 30, 2024.. Amid an unexpectedly large surge of summer COVID infections in the U.S., and with the fall/winter virus season around the corner, updated COVID vaccines have arrived.. COVID vaccines are one of the best and safest ...
Uganda Level 3 - Reconsider Travel C T O. Reissued with updates to terrorism information. Reconsider travel to Uganda due to crime, terrorism, and anti-LGBTQI+ legislation. Some areas have increased risk. Read the entire Travel Advisory. Country summary: There remains a threat of terrorist attacks in Uganda and throughout the region. Numerous ...
The Ministry of Health's long COVID programme develops clinical guidance and funds research to help support people with long COVID in New Zealand. More east. More. Behavioural science research. Access research on people's attitudes and behaviours to the COVID-19 pandemic commissioned by the Ministry of Health.